37year old patient with abdominal distension and fever
is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
CASE PRESENTATION:
A 37 year old female patient house wife by occupation came with chief complaints of abdominal distension and fever from 5days.
HOPI:
Patient was apparently asymptomatic 5days ago then developed Abdominal distension and fever 5days back. Low grade intermittent fever not associated with chills and rigors.
H/O abdominal distension from 5days insidious onset gradually progressing.
H/O polyuria and generalised weakness
No H/O chest pain , palpitations,jaundice,melena, pedal edema , giddiness.
PAST HISTORY:
4 years ago patient had complaints of jaundice and pain abdomen for one month , usg abdomen was done which showed altered echo texture of liver , gross splenomegaly with multiple vascular channels at splenic hilum , mild ascites, right minimal pleural effusion .
She underwent splenectomy for which no records were available and the patient or her attenders were not clearly explained about the need for splenectomy.
Not a known case of HTN and DM.
PERSONAL HISTORY:
Normal appetite
Adequate sleep
Addictions:toddy drinker
Mixed diet
GENERAL EXAMINATION:
Patient is conscious coherent co-operative Oriented to time,place and person
Moderately nourished and moderately built.
VITALS:
Patient is afebrile
BP :160/100mm hg
Pulse rate : 72bpm regular
RR : 22 cpm
SYSTEMIC EXAMINATION:
Per abdomen - distended.
CVS: S1 S2 Heard no murmurs
RS: BLAE present NVBS
CNS : No abnormality detected
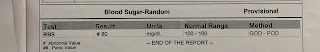
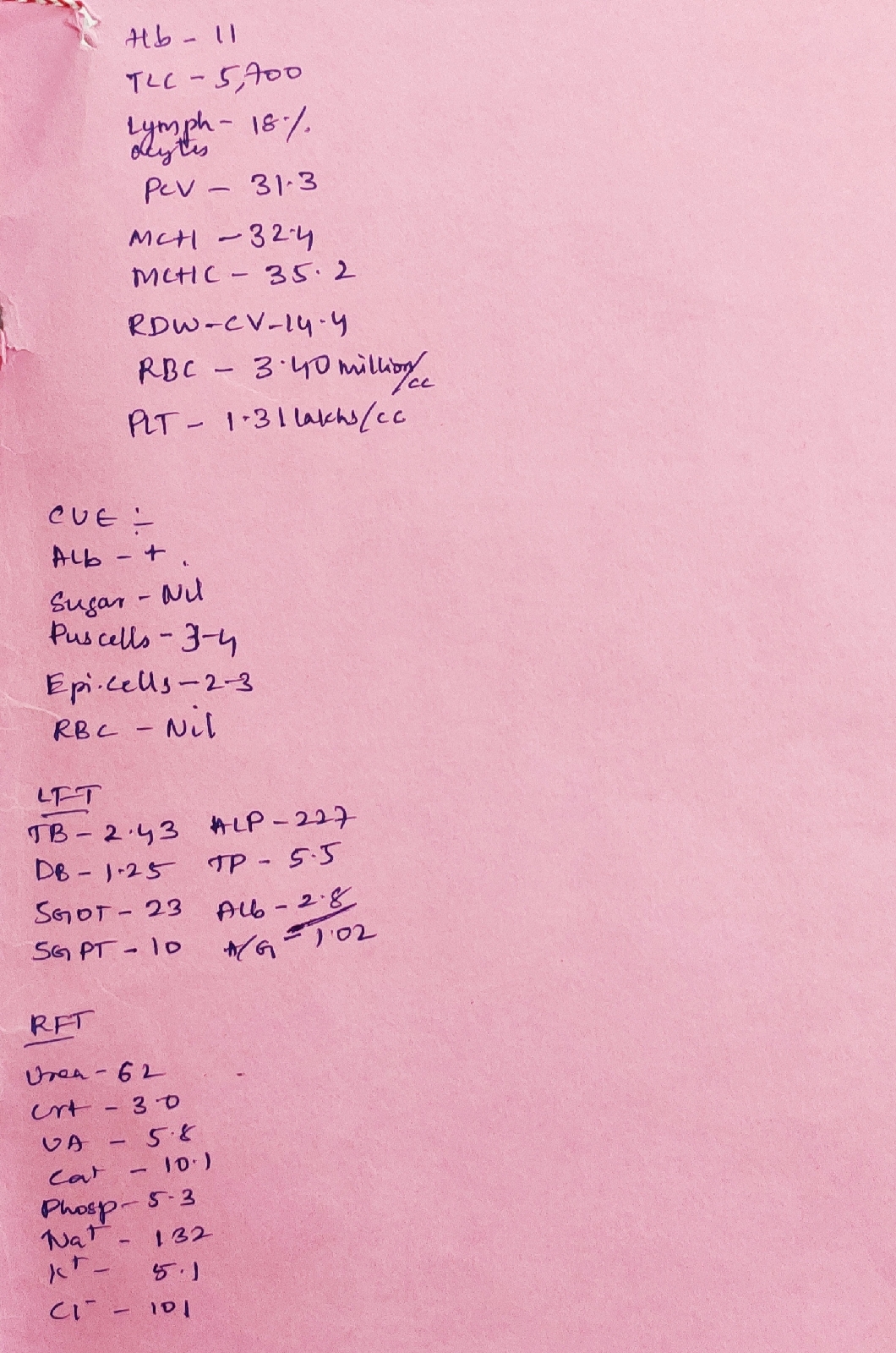
INVESTIGATIONS :
5/11/2020
Aptt-30secs
6/11/2020
Peripheral smear:
RBC- anipoikilocytosis with microcytes , tear drop cells , pencil forms , target cells and schistocytes.
WBC - neutrophilic leucocytosis
PLATELETS- adequate
IMPRESSION - Microcytic hypochromic anemia with neutrophilic leucocytosis
SEROLOGY - Negative
ASCITIC FLUID ANALYSIS
Serum albumin-2.8gm/dl
Ascitic albumin - 0.31gm/dl
SAAG - 2.49
LDH - 41.3IU/L
Amylase - 11.1IU/L
Sugar - 91mg/dl
Protein-0.5gm/dl
Fundoscopy - normal fundus no KF Ring seen on slit lamp examination
2D ECHO:
Mild mitral regurgitation, mild triicuspid regurgitation with PAH
Trivial aortic regurgitation
No RWMA
No AS, MS
Good LV Systolic function and no diastolic dysfunction.
USG Abdomen:
Impression- chronic liver disease
Cholelithiasis
Gross ascites
Left kidney grade 1 RPD changes.
DIAGNOSIS:
ASCITES SECONDARY TO CHRONIC LIVER DISEASE
SEVERE ANEMIA , DENOVO HYPERTENSION.
TREATMENT:
Day 1
Fluid restriction less than 1.5lit per day
Salt restriction less than 2.5gm/day
Tab lasilactone 20/50 PO OD
Tab nicardia 20mg PO STAT
Vitals,input and output monitoring
Day 2
Fluid restriction less than 1.5lit per day
Salt restriction less than 2 gm per day
Tab lasicactone 20/50 PO OD
INJ zofer 4mg IV SOS
INJ pantop 40mg IV OD
Vitals monitoring
Day 3
Fluid restriction less than 1.5lit per day
Salt restriction less than 2 gm per day
Tab lasicactone 20/50 PO OD
INJ zofer 4mg IV SOS
INJ pantop 40mg IV OD
Tab rifagute 550mg PO BD
SYP Hepamerz 10ml PO BD
Tab Cilindepine 10mg PO OD